Medical Decision-Making

Medical Decision-Making
Our decision-scientists, physicians and researchers examine evidence-based outcomes using data and cost-effectiveness analyses to promote better health policy outcomes. Working closely with the Society for Medical Decision Making, SHP researchers propose standards to help guide physicians and their patients, as well as state and federal policymakers who set those standards in legislation. Many of our faculty are also investigators and clinicians at the VA Palo Alto Health Care System and have published hundreds of studies in medical journals about the best clinical practices.
Vaccines and Public Health in an Era of Distrust
Health Policy Forum: Two leading vaccine experts discuss the future of vaccines and public health in an era of widespread distrust.
Vaccines and Public Health
Evidence-Based Decision Making During Pandemic
Doug Owens on New Statin Recommendation
Keith Humphreys: Is Addiction a Disease?
Rosenkranz Prize Honors Innovators Tackling Public Health in Mexico
Two Stanford researchers, including SHP"s Fernando Alarid-Escudero, win the 2025 Rosenkranz Prize for their bold public health efforts in Mexico—tackling the urgent threat of antimicrobial resistance and designing a national colorectal cancer screening program for those most at risk.
Meet the Winners
Health-Focused Arguments for Eliminating Overcrowding in Prisons
Jeremy Goldhaber-Fiebert writes in this commentary that overcrowding at U.S. prisons and jails not only leads to negative health outcomes for individual residents, but exacerbates chronic physical and mental health conditions and increases demands for already limited healthcare delivery.
Read Story
How to Know When a Doctor’s Age Might Compromise Their Practice
A paper co-authored by Stanford Law School’s Michelle Mello examines policies that health-care organizations are implementing to address potential risks associated with cognitive and physical decline in late-career physicians (LCPs).
Read Stanford Report Story
TB Continues to Prey on Underserved US-born Americans
In a new study by members of Josh Salomon's Prevention Policy Modeling Lab, the researchers found profound racial and ethnic disparities that are stalling overall progress against TB.
Go To Story
Modeling Lab Awarded CDC Grant To Examine Effectiveness of US Disease Prevention
The Prevention Policy Modeling Lab (PPML) led by SHP's Josh Salomon has been awarded a five-year grant from the Centers for Disease Control and Prevention (CDC) to continue evaluating the health impact, costs and cost-effectiveness of infectious disease treatment and prevention programs in the United States.
Go To Story
Promoting Diabetes Translational Research in Health Equity
DREAMS Center for Diabetes Translational Research, co-directed by SHP's Alyce Adams, holds national enrichment program meeting to draw early stage investigators focused on diabetes equity research.
Go to Story
QALY Ban Could Harm People with Disabilities and Chronic Illness
The U.S. House passed a bill that would ban the use of a metric known as quality-adjusted life-years (QALYs) in coverage and payment determinations for federal health-care programs. SHP's Joshua Salomon writes in this Health Affairs commentary the bill would compromise the evaluation of medical treatments.
Go To Story
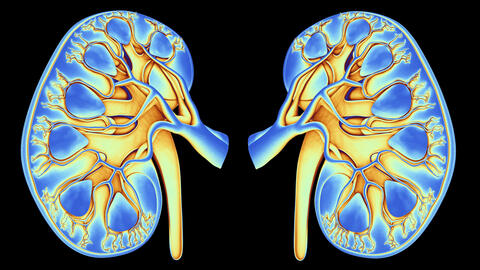
Removing Race Adjustment in Chronic Kidney Disease Care
A new study led by Stanford Health Policy researchers finds that algorithmic changes to a chronic kidney disease care equation are likely insufficient to achieve health equity as many other structural inequities remain.
Go To Story